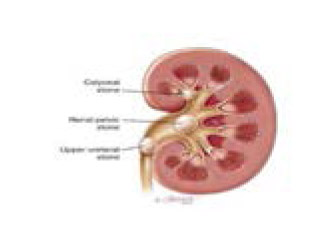
For the kidney to be able to work properly the following are required:
- A supply of blood that needs to be cleaned
- A cleaning or filtration system to clean the blood
- A way for the cleaned blood to return to the rest of the body
- A way of allowing excess water and waste to leave the kidney and then the body
Your kidneys need all four conditions to work properly. If this is not so, then urine is not produced by the kidneys and waste is not removed from the body properly. If the blood has not been cleaned when it returns to the body, waste products will accumulate and certain organs and tissues begin to be harmed. Eventually this results in illness which is generally known to as “kidney disease”. There are many different causes of kidney disease.
Examples where things can go wrong and cause kidney disease include:
- No blood supply to the kidney - the blood will not be filtered and cleaned. This can occur when the arteries supplying the blood to the kidneys become narrowed
- Blood is supplied to the kidneys but the filtration systems are not working - the blood will pass out of the kidney again, just as it went in, so no waste will have been removed. This can occur when the kidney is damaged by diseases such as “nephritis”
- When the blood has been filtered and urine made, but does not pass out – the waste products will remain in the body. This may occur as a result of a blockage (obstruction) to the tubes which drain urine from the kidney to the bladder or from the bladder to the outside. If the blockage is not relieved the kidneys will swell up and stop working
Renal failure occurs when the kidneys fail to function properly. Normally, your kidneys work continuously to keep you alive and well. They act as filters and remove waste products from the blood and excess water from your body.
High blood pressure (hypertension) is both an important cause and consequence of kidney disease. Indeed, for some it can be difficult to determine which came first. In those with kidney problems controlling high blood pressure is the most important measure that can be taken to reduce the risk of progressive kidney damage. Treatment of hypertension is therefore very important as it also reduces the risk of cardiovascular problems such as heart attacks and strokes.
Early detection and diagnosis is important, so treatments can begin sooner. ‘Screening’ is an initiative that encourages people to come forward for a kidney health check. The sooner any problems are discovered, the better.
The management of kidney disease depends on the severity of kidney damage found. This is graded in stages one to five, depending on how impaired the kidneys are.
- In the early stages (CKD 1-3) important issues are lifestyle adjustments, treatment of diabetes (if present) and good control of blood pressure
- In more advanced CKD (stage 4-5) specific treatments for the effects of kidney disease are required and are frequently provided by “pre-dialysis” or “low clearance” programmes
- When very advanced (end stage kidney failure) (stage 5) renal replacement with either dialysis or transplantation should be considered. However, not everyone will benefit from renal replacement and this decision needs careful discussion between each person and their kidney team
Increasingly, the earlier stages (one to three) of renal failure are managed at the local doctor’s surgery by the GP team.
The treatments are simple – they focus on protecting renal function by the promotion of good health and lifestyle.
Treatments include the management of blood pressure and any diabetes (if it exists.) Attention is given to lifestyle – you will be encouraged to eat healthily, reduce your salt intake, become more active, exercise and stop smoking, if you haven’t already. Attention will be given to your general health also.
Your doctors will measure your blood pressure and take urine and blood tests regularly to make sure your condition has stabilised.
If your renal failure looks as though it is going to progress beyond stage 3, your GP will refer you to a kidney specialist (nephrologist or renal physician) at your nearest renal unit.
Renal Units have teams of specialist staff to help with all forms of treatment for kidney disease, including dialysis and transplantation.
The teams consist of doctors, surgeons, renal nurses, laboratory scientists, transplant co-ordinators, dieticians, social workers, counsellors, renal technicians and others as required. They will all work together to provide treatment, advice, training and support, be it physical, psychological or financial - even arranging transport requirements to and from treatments Their objective is to give kidney patients and their family the most up-to-date treatment and support available so they can return to as independent a lifestyle as possible.
Dialysis is a mechanical substitute for lost kidney function. When the kidneys fail to work efficiently renal failure develops, and eventually dialysis is required as a matter of priority to take over the kidney function, and so maintain life.
Dialysis will be necessary if you reach ‘end stage renal failure’. Though the expression may sound dramatic, it simply refers to your renal function reaching the point where you need to start dialysis to maintain good health.
Advice is always given on which of the two methods will suit you best and there be opportunity to look at both and ask as many questions as you like.
You can change your mind at a later stage and opt for a different treatment if it is clear that a change will improve your wellbeing, both medically and socially.
Some people find that hospital environments depress them. In dialysis centres staff have created an environment that is as welcoming, cheerful and friendly as possible. Attractive décor, televisions, piped music and an efficient but relaxed ambience will help make you feel comfortable during your treatment.
My Grandfather was suddenly admitted to hospital as his kidneys have stopped working. I have heard that he has something called a 'temporary access' for his dialysis while he waits for a 'permanent access' to be made. I am confused why will he need a temporary and then a permanent access? Why can't he have just the one?
Usually, when someone needs dialysis, enough time for preparations need to be made. This includes time for the preparation of a fistula which will help someone have their dialysis more conveniently. This is a direct connection between vein and artery, beneath the skin. A fistula can take up to 3 months before it is ready for use, although it usually ready in 6 to 8 weeks for permanent use.
Some people find that hospital environments depress them. In dialysis centres staff have created an environment that is as welcoming, cheerful and friendly as possible. Attractive décor, televisions, piped music and an efficient but relaxed ambience will help make you feel comfortable during your treatment.
The fistula
The fistula is formed by connecting a vein and artery to form a larger, more robust blood vessel. This surgery is done in theatre under local or general anaesthesia. In some cases, a special exercise is given that will help to build up the veins in the arm. This is started before surgery and carried on afterwards for about 3 months. Meanwhile the swelling goes down as the walls of the fistula thicken, blood flow increases and the fistula heals. Occasionally though, dialysis has to be given quickly, in order to save someones life.
Temporary Access
A catheter, known as a line is used for short term dialysis, perhaps while a fistula is being prepared. This is a soft, flexible tube which is placed in a large vein of the neck, chest or groin under local anaesthesia. This is stitched in place and as a dressing that is changed at dialysis session. Different types of catheter are suited to the different access sites and again, some catheters are designed for 48 hour use ranging through to those that can be used for several months. The longer term use catheters are designed to be comfortable and to reduce complications.
There are two types of dialysis - HAEMODIALYSIS and PERITONEAL DIALYSIS.
- Haemodialysis and peritoneal dialysis both require a form of access
- Haemodialysis is the removal of waste material and water using an artificial kidney linked to a dialysis machine
- It is mainly done at hospital but can take place at home
- Peritoneal dialysis uses the natural membrane in the abdomen called the peritoneum for dialysis
- This type of peritoneal dialysis used is called CAPD - Continuous Ambulatory Peritoneal Dialysis
- This form of dialysis takes place at home only and gives the patient greater freedom in their lifestyle
A BLOOD ACCESS is necessary for haemodialysis. It is called a fistula, which is a vein and artery surgically joined together under the skin, usually in the patient’s forearm. Once formed, this fistula needs to develop for ease of use, so it needs to be formed sometime in advance. If dialysis is required as an emergency then other forms of blood access are available for use in the short term.
A PERITONEAL ACCESS involves a soft tube being inserted permanently into the patient’s abdomen for the purpose of dialysis. This means that the patient has complete freedom to walk around and continue normal home and work activities.
The major change in diet is a reduction in the foods high in potassium and sodium (salt). In addition a restriction of fluid intake may be required and this can be very difficult for dialysis patients.
Diet will have to carefully adjusted for each individual, and certain foods will be restricted. Fluids will also be restricted according to each person’s requirements. A dietician specialising in renal nutrition will provide the patient and their family with all the information required on the kind of food and fluid recommended and how to prepare it.
According to the type of employment, some flexibility is needed to fit work around dialysis requirements Others may find they have to give up work altogether in the short term. If necessary, your social worker and community dialysis sister will (with your permission) talk to your employer about your treatment to help alleviate any concerns you may have, as well as those of your employer. The dialysis unit will do all they can to arrange your treatment times so that they fit in with your work schedules.
Financial worries can be discussed and, where applicable, certain benefits applied for, such as mobility and disability living allowance. The renal social worker also has access to certain kidney patient organizations that can provide assistance or act as a support group for you and your family.
Dialysis places a considerable strain on personal relationships, often making communication between you and your partner difficult. This, in turn, may have a knock-on effect on those around you. Many of those on dialysis and their families find that meeting with others in a similar position is a great help and support. Most renal units will have an active patients group.
When considering pregnancy there are several things that a woman may consider:
- Will my pregnancy be complicated?
- Will kidney disease affect my baby?
- Who will look after me in pregnancy?
- Can I deliver my baby normally?
- Will pregnancy make my kidney disease worse?
Such questions are best asked before you get pregnant. Speak to your family doctor, an obstetrician, a kidney doctor or a specialist nurse. If your kidney disease is mild then the chance of a successful pregnancy is good. By knowing what to expect you can make an informed choice about pregnancy for yourself.
I have Kidney problems and high blood pressure. I know this will make my kidney problems worse. How can I reduce my high blood pressure?
People with a long-term raised blood pressure are at risk of damage to heart and blood vessels. This means they will be more likely to have heart attacks and strokes.
Kidney problems are aggravated by high blood pressure. Treating blood pressure slows worsening in many kidney conditions and is the most important way of reducing progression towards kidney failure for many conditions. The following actions will help:
Avoid being overweight
Being too heavy increases your blood pressure. Try to eat a low fat, high fibre diet and aim to consume five portions each day of fresh fruit and vegetables if this is appropriate for your kidney diet. Your dietician will be able to guide you.
Keep alcohol consumption to a sensible level
Your alcohol consumption should be spread evenly over the week following the health recommendation of 21 units for men and 14 for women.
Reduce salt intake
Blood pressure is increased by a diet that is high in salt. Salt content is not always obvious and is contained within many processed foods. It is best not to add salt and to eat plenty of fresh, unprocessed foods.
Exercise regularly
Exercise can help you reduce your weight and your blood pressure. Try to aim for at least 3 sessions a week of 20-30 minutes each, that will make you a little breathless.
Stop smoking
Stopping smoking not only lowers your blood pressure, it reduces the risk of heart attack and stroke as there is less smoking related damage to the blood vessels.
For every diabetic patient precaution for the prevention of kidney disease is essential because diabetes is the leading cause of chronic kidney disease (CKD) and kidney failure throughout the world. About 45% of new cases of end stage kidney disease are due to diabetic kidney disease.
High blood pressure, presence of protein in urine, swelling, frequent reduction of blood sugar, reduction in insulin requirements and appearance of diabetic eye disease (diabetic retinopathy) areimportant clues of kidney involvement in diabetes. Beware of these danger signals and consult your doctor.For early diagnosis of diabetic kidney disease, a simple and effective way is three-monthly measurement of blood pressure and urine test to check for the presence of protein
by dipstick (macroalbuminuria).The best and ideal test for the earliest diagnosis of diabetic nephropathy is the urine test for microalbuminuria (MA), which should be done every year. Measure blood creatinine (and eGFR) to assess kidney function at least once every year.
To prevent diabetic kidney disease all diabetics should control diabetes meticulously, maintain blood pressure less than 130/80 mm. of Hg and control lipids.
Kidney transplantation is the treatment of choice for end-stage kidney disease (ESKD). Successful kidney transplantation may offer better quality of life and longer patient survival compared with dialysis. Kidney transplantation is a surgical procedure in which a healthy kidney is placed into the body of a person suffering from end-stage kidney disease (recipient).Life after successful kidney transplantation is almost normal.
kidney transplantation offers the best treatment option for complete rehabilitation of a patient with end-stage kidney failure. As kidney transplantation saves lives and enables one to enjoy almost normal life, it is referred to as the “Gift of Life”.
A healthy person with two kidneys can donate one kidney as long as the blood group, tissue type and tissue crossmatching are compatible with the receipient. Generally, donors should be between the ages of 18 and 65 years.
A living donor should be thoroughly evaluated medically and psychologically to ensure that it is safe for him or her to donate a kidney. A person cannot donate kidney if he or she has diabetes mellitus, cancer, HIV, kidney disease, high blood pressure or any major medical or psychiatric illness.Risk of contracting kidney disease in kidney donors is not any higher just because they have only one kidney. After kidney transplantation, lifelong regular medications(Immunosuppressant) and meticulous care are mandatory.
Deceased (cadaver) transplantation involves transplanting a healthy kidney from a patient who is “brain dead” into a patient with CKD. The deceased kidney comes from a person who has been declared “brain dead” with the desire to donate organs having been expressed eitherby the family or by the patient previously, at the event of his/her death.Giving another person a new lease on life is an invaluable gift.
Maintain a healthy fluid intake:*
Drink 8-10 glasses of water each day. “Start the day by drinking a glass of water and offer one to visitors”
Manage blood pressure:
If you have Hypertension, Go for regular BP checkup and Keep your blood pressure in normal range (below 140/90 mmHg).

Keep your blood sugar level under check:
If you have diabetes, monitor your blood glucose levels and kidney function regularly.
Ward off kidney stones:
If you have renal stone disease, treat it on urgent basis

Do not take over-the-counter pills on a regular basis:
Excessive intake of over-the-counter pills, painkillers and analgesics such as ibuprofen can damage your kidneys.
Live an active Life:
Be more physically active and exercise regularly.
* This information is for person with normal kidney function. Kindly consult to your doctor if you have kidney problem.
Get your kidney function checked if you have one or more of the ‘high risk’ factors
- you have diabetes
- you have hypertension
- you have renal stone disease
- you have recurrent UTI
- one of your parents or other family members suffers from kidney disease
- you are obese
